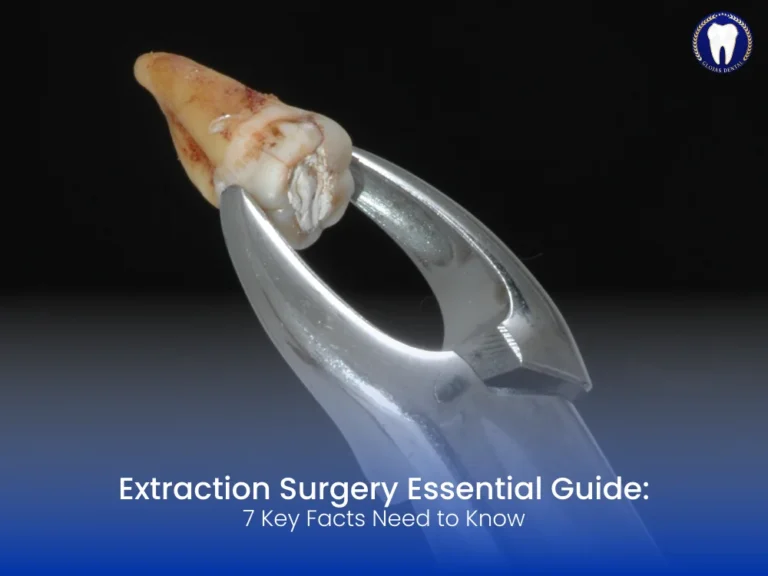
When it comes to dental health, extraction surgery is often seen as a last resort—but sometimes it’s the most essential step toward a healthier, pain-free mouth. Whether it’s due to impacted wisdom teeth, severe decay, or orthodontic preparation, extraction surgery plays a crucial role in modern dentistry.
In this article, we’ll explore the 7 key facts you should know about extraction surgery, from understanding when it’s necessary to how to prepare and recover like a pro. This guide is ideal for patients seeking accurate, and reassuring dental content.
What Is Extraction Surgery?
Extraction surgery refers to the surgical removal of a tooth that cannot be extracted through simple means. Unlike routine extractions, surgical extractions are more complex and often involve cutting into the gum or bone to fully remove the tooth. This is common with impacted wisdom teeth, broken teeth, or teeth with curved roots.
When Is Extraction Surgery Necessary?
Impacted Wisdom Teeth
Wisdom teeth that do not erupt properly often cause pain, swelling, or infection. Extraction surgery is necessary when these teeth are stuck under the gum or are growing at an angle.
Severe Tooth Decay or Infection
When a tooth is too damaged to be restored with a crown or root canal, surgical extraction may be the only viable option to prevent the spread of infection.
Orthodontic Treatment
In some orthodontic cases, dentists recommend extraction surgery to create space for aligning the remaining teeth.
Broken or Fractured Teeth
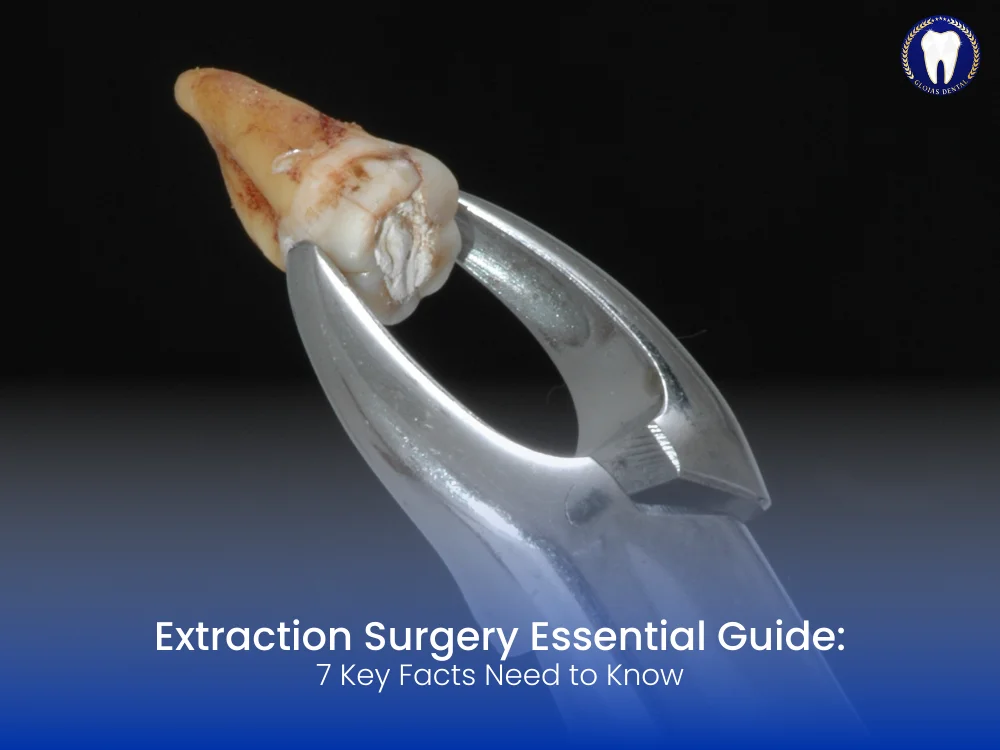
If a tooth is broken below the gum line, surgical extraction is required as it cannot be pulled out using standard tools.
Types of Extraction Surgery
Simple vs. Surgical Extractions
- Simple Extraction: Performed on visible teeth using forceps.
- Surgical Extraction: Involves incision into the gum and possibly bone removal.
Soft Tissue Extraction
Used when the tooth has partially erupted through the gum.
Partial Bony Extraction
Needed when part of the tooth is encased in jawbone.
Full Bony Extraction
Most complex type, performed when the tooth is completely embedded in bone.
The Extraction Surgery Procedure
Initial Consultation
Your dentist or oral surgeon evaluates your condition using X-rays and medical history.
Anesthesia
Local anesthesia, sedation, or general anesthesia is administered depending on the complexity of the case.
Surgical Process
The surgeon makes a precise incision, removes bone if necessary, and extracts the tooth. Sutures may be placed to aid healing.
Recovery After Extraction Surgery
Immediate Aftercare
- Bite down gently on gauze to stop bleeding.
- Apply ice packs to reduce swelling.
- Avoid rinsing or spitting forcefully.
Pain Management
Prescribed pain relievers or over-the-counter medications help manage discomfort. Avoid aspirin as it may increase bleeding.
Diet Adjustments
Stick to soft, cold foods like yogurt, smoothies, and mashed potatoes for the first 24-48 hours.
Oral Hygiene
Gently brush teeth around the surgical site and use a saline rinse after 24 hours to keep the area clean.
Risks and Complications of Extraction Surgery
Dry Socket
Occurs when the blood clot dislodges, exposing nerves and causing severe pain.
Infection
Signs include fever, pus, or prolonged swelling. Antibiotics may be needed.
Nerve Damage
Rare but possible in lower wisdom teeth surgeries. It may cause numbness or tingling in the lips, chin, or tongue.
Excessive Bleeding
Should subside within 24 hours. If it doesn’t, contact your dentist immediately.
How to Prepare for Extraction Surgery
- Provide Full Medical History including medications and allergies.
- Avoid Eating/Drinking 6–8 hours before surgery if undergoing sedation.
- Arrange Transportation if you’ll be sedated or under general anesthesia.
- Follow Pre-Op Instructions given by your dental professional.
What to Expect Post-Surgery
Swelling and Bruising
Mild to moderate swelling is normal and peaks within 48 hours.
Minor Bleeding
Gums may bleed for a few hours; bite down on clean gauze to control it.
Restricted Activity
Limit strenuous activities for at least 24–48 hours post-surgery.
Long-Term Oral Health After Extraction Surgery
Removing problematic teeth through extraction surgery can improve overall dental health, prevent future infections, and aid orthodontic treatments. Once healed, dental implants or bridges can replace the missing tooth to restore function and aesthetics.
Myths About Extraction Surgery
“It’s Always Painful”
Thanks to modern anesthesia, most patients experience minimal pain during the procedure.
“You Lose Bone Forever”
While bone loss can occur, socket preservation techniques can maintain bone density.
“Recovery Takes Weeks”
Most people recover significantly within 7–10 days with proper aftercare.
FAQs About Extraction Surgery
1. Is extraction surgery painful?
With the use of local anesthesia or sedation, the procedure itself is usually painless. Some discomfort may occur post-surgery, which is manageable with pain medication.
2. How long does extraction surgery take?
On average, the procedure lasts 20 to 40 minutes, depending on the complexity.
3. Can I go back to work after extraction surgery?
It’s best to rest for at least 24 hours post-surgery. Most people return to work within 2–3 days.
4. When can I eat normally after extraction surgery?
Soft foods are recommended for the first 48 hours. You can gradually return to a regular diet based on comfort and healing.
5. What should I avoid after extraction surgery?
Avoid smoking, drinking through straws, spicy foods, and rigorous rinsing for at least 48 hours.
6. Can I brush my teeth after extraction surgery?
Yes, but avoid the surgical site for the first 24 hours. Brush gently around the area to maintain oral hygiene.